Testing for gluten sensitivity can be a frustrating struggle, and some say there isn't a test. This is our family's testing story that began two years ago.
Here is a quick description of how it works. Wheat, barley, and rye contain gluten, more specifically, a class of proteins called gliadin. The experts say we cannot digest this, and it makes some people sick. I think of it as a war going on inside your body: When you are eating gluten, your body responds by sending out troops to fight it. These troops are the antibodies. The tests for gluten sensitivity measure your antibody levels, some of which are called IgA and IgG. That is a very simple explanation to a complex chain reaction.
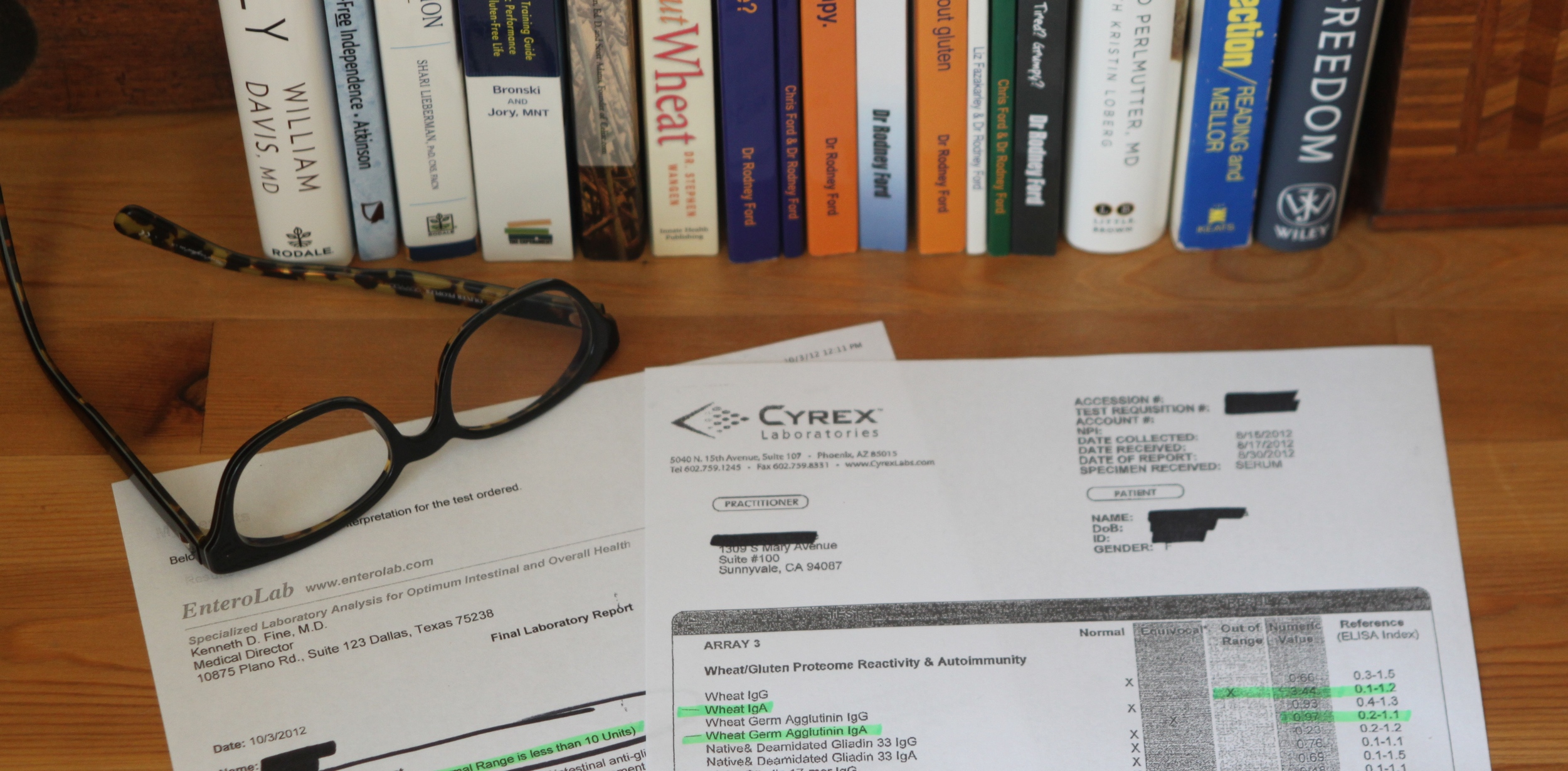
I was a patient at HealthNOW Medical Center a few years ago and had the blood test from Cyrex Lab. Cyrex tests for many different proteins within gluten. My results showed I had elevated antibodies to several proteins in gluten. I was diagnosed with gluten sensitivity and immediately went on a gluten-free diet. The doctor made clear that gluten sensitivity can be genetic, and my family members should be tested.
Our daughter, who was 8-years old at the time, wouldn’t do the blood test, so she had a stool test by Entero Lab. Her results came back positive for gluten sensitivity, and her numbers were the highest the doctor had seen in a child.
My husband decided he should be tested too as our daughter now had the diagnosis, and he suffered from IBS (Irritable Bowel Syndrome). He used the Cyrex test, and his levels were just barely elevated. This still meant he was gluten sensitive, even though his antibody numbers were only slightly high. I wanted to “test the tests,” so I had my husband also do the Entero Lab stool test. The results were clearly positive for gluten sensitivity. He immediately went gluten-free.
My parents simply stopped eating gluten after my test results came back positive as they understood the genetic connection. In addition to that, they also wanted to be supportive and have a gluten-free kitchen that was safe for our family when we visited. They are wonderful! But, I wanted them to be officially tested as part of my understanding and research. The medical community agrees it is essential to be eating gluten before you have a test, so Mom and Dad begrudgingly started eating gluten again, which made them feel awful. They didn’t have access to the Cyrex test and used the Entero Lab stool test.
My mother’s test results had just enough elevated antibodies to diagnosis gluten sensitivity. She stopped eating gluten and was eager to start feeling better. She had already experienced symptom relief the first time she went gluten-free after my diagnosis, so she knew good things were ahead.
My father’s antibodies weren’t elevated enough to diagnosis gluten sensitivity. My parents' primary care physician, who recognizes gluten sensitivity as a real condition, was mystified because he thought for sure the results would be positive based on my father’s symptoms and my results. The tests, however, are not flawless. False negatives happen. Also, some people don’t produce high amounts of antibodies to begin with, and it’s possible their immune system is worn down and has gotten tired of sending out the troops (antibodies). My dad, who was 77 at the time, understood these variables and immediately went gluten-free again. He is the example of having a negative test result but proving gluten sensitivity just by feeling better on a zero gluten diet. Read about my father’s recovery from years of lichen planus disease and his fingernails growing back after going gluten-free! Isn’t it ironic that my dad had the lowest level of antibodies (not enough to “diagnosis”) but the most dramatic improvements in his health after going gluten-free?
Six weeks after I was diagnosed with gluten sensitivity, I was tested for celiac disease by my primary care physician at another medical center. It was recommended that I have a traditional celiac blood test rather than a bowel biopsy. A blood panel was ordered that tested my IgA antibody levels only, and the results were negative. I didn’t know at the time that I should have requested my IgG antibody levels also be tested. In addition, I had been gluten-free for six weeks and had been taking steroids after a tonsillectomy; all of which flawed the results. A year later I saw two gastroenterologist specialists who stated that based on my varied and severe symptoms, I probably had celiac disease. Either way, my future was going to be gluten-free, or “gluten zero” as Dr. Rodney Ford prefers to call it.
My daughter, husband, and parents weren't tested for celiac disease. We will never know if they have it because one must be eating gluten when you take the test. And, there is no way they will eat gluten again because it makes them so sick...it’s not worth it.
Listed below are a few resources to learn more about gluten testing. Dr. Rodney Ford has been studying the effects of gluten in his clinic for over 30 years. His website is set up to educate doctors (and patients), and in my opinion, it is the best resource. Dr. Ford outlines the fine details of blood testing for celiac disease and gluten sensitivity.
- Dr. Rodney Ford's website
- Dr. Alessio Fasano’s book, Gluten Freedom
- Dr. David Perlmutter’s book, Grain Brain
Our family’s test results were the beginning of our gluten-free journey. The long list of health ailments that plagued us began to disappear, and our bodies started the healing process. We are so much happier!
I've written numerous blog posts about my family's diverse gluten symptoms and created a category called Gluten Symptoms on my website. Scroll through the older posts to learn more, and I hope this helps.